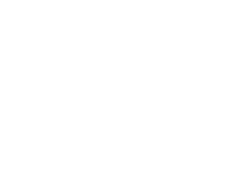
Dr. Shantanu Agrawal on Combating Fraud, Waste & Abuse in Healthcare
The U.S. was projected to spend $3.1 trillion dollars on healthcare generating billions of claims from healthcare service and product providers every year. Medicare alone accounts for something on the order of $635 billion in annual spending. Given the level of spending and resource allocation, protecting the integrity of government healthcare programs, such as Medicare, Medicaid, and Children's Health Insurance Program (CHIP), is a key priority for the Centers for Medicare and Medicaid Services (CMS), the agency within the Department of Health and Human Services (HHS) responsible for the Medicare program. The Center for Program Integrity is the division within CMS that serves as the primary agent for combatting fraud and abuse. “The Center was created just before the passage of the Affordable Care Act,” says Dr. Agrawal, “but the ACA gave the Center far more expanded authorities and much of our efforts derive directly from the ACA.” Collaborating with other HHS components and the Department of Justice, the Center for Program Integrity develops and implements a comprehensive strategic plan, objectives and measures to carry out CMS’s Medicare, Medicaid and CHIP program integrity missions and goals, and ensure program vulnerabilities are identified and resolved. The Center’s efforts have borne fruit. On February 26, 2014, HHS and DOJ jointly announced the recovery of $4.3 billion in FY 2013 by reflecting a return of $8.10 on every dollar spent on fraud detection and prevention, the highest rate in the program’s 17-year history. This is no easy feat to achieve. Dr. Agrawal provides his insights on the challenges faced, the strategic priorities pursued, and the many ways CPI both prevents and combats fraud, waste, and abuse in federal healthcare programs. On Challenges Ensure Coordination - Challenge number one is ensuring successful coordination of our efforts across the department and with other federal agencies. I've seen among CMS leadership a real willingness to do that and build on that coordination, which has aided my efforts. Identify Real Vulnerabilities -- The second challenge has its roots in the volume and size, the sheer magnitude of the programs. We need to make sure we’re not overwhelmed by this reality. We need to understand how to prioritize the various issues we encounter. It is a challenge making sure that we are going after issues that represent real vulnerabilities, which if successfully addressed, can lead to real savings, savings which then can be used for provide legitimate healthcare services for our beneficiaries. Balance Means with Ends - Finally, I think we need to make sure we address program vulnerabilities with the right tools at our disposal. It is a matter of balancing end and means. We need to secure the integrity of our programs. We need to do this without overly burden the very legitimate physicians and providers that we have in our system that are seeing our patients that are offering the necessary healthcare services. I think it’s a very difficult balance to achieve. Meeting these challenges head on involves pursuing key strategic priorities. Dr. Agrawal highlights his priorities. On Key Strategic Priorities Provider enrollment screening standards -- We've integrated literally hundreds of databases to give us access to right-time information so we can check provider eligibility both at the time of enrollment and post-enrollment to ensure providers are maintaining their eligibility. We receive about 10,000 enrollment applications per month -- not a trivial task. This year we are also focusing on enrolling providers, who may want to simply prescribe medication under Medicare and bill no other kinds of services. Program integrity education, training, & collaboration -- There are several initiatives we are pursuing around education and training. The Medicaid Integrity Institute (MII) provides a unique opportunity for CMS to offer substantive training, technical assistance, and support to the States in a structured learning environment. The mission of the MII is to provide effective training, tailored to meet the ongoing needs of State Medicaid program integrity employees, with the goal of raising national program integrity performance standards and professionalism. We're also providing similar services directed at the private sector through our public private partnership. On the other side, we'll continue expand our outreach and education with providers to make sure they're aware of our policies and collaborate on remedying issues we all care about. Again, the vast majority of providers are doing the right thing. They're taking care of patients and we need to preserve that a relationship, but we also need to weed out those bad actors while we collaborate with those whose intentions are good, but for whatever reason seem to be missing the mark when it comes to documentation. We are also looking to conduct similar activities with private payers – many of the same issues and vulnerabilities that we experience are also experienced by the private sector. We're working more closely now with the private sector to try to close those vulnerabilities across the entire healthcare system. Advanced predictive analytic -- Data is essential to what we do. We have implemented a state-of-the-art predictive analytics technology -- the Fraud Prevention System (FPS). Since June 2011, the FPS has run predictive algorithms and other sophisticated analytics nationwide against all Medicare fee-for-service (FFS) claims prior to payment. For the first time in the history of the program, CMS is systematically applying advanced analytics against Medicare FFS claims on a streaming, nationwide basis as part of its comprehensive program integrity strategy. CMS made significant progress using the FPS to identify bad actors and take administrative action to protect program integrity. With FPS, we work every day trying to realize saving, but it's not only more identified savings we've also taken some significant actions as a result of the system. Over 900 providers have faced some kind of administrative action, either starting a new investigation or audit or supplementing something that already existed. Timely and efficient action -- A priority of mine is really to focus on timely and efficient action. We have to focus on the right vulnerabilities and issues. We have to use the right tools at our disposal to address these issues and focus on meeting outcomes. I don't like the notion of interminable audits or endless investigation. It's burdensome on providers. Let's take the most appropriate actions that address the weakness of vulnerabilities for it is our job to ensure the integrity of these programs. On Shifting Away From Pay and Chase In combating fraud, waste, and abuse, we’ve prioritized moving away from a “pay and chase” model to a prevention model. The “pay and chase” model is fraud driven and again there is fraud in the system, which we take seriously as it is criminal activity. That said, we must also have to focus on prevention, making sure we reduce waste in the healthcare system while also driving patient value. Jettison nearly 50,000 providers who didn’t belong in the system because they failed to meet our requirements is a good example of a prevention strategy at work. We no long need to pay providers who have no business collecting payments, and therefore, won’t have to chase down improper payments from these ineligible providers On the Future The shift from the current fee for service system to one that really prioritizes quality outcomes and value is absolutely the right shift. It's right for many reasons beyond just program integrity. It's right for American healthcare, for patients, and ultimately right for providers. This shift would deemphasize focusing on specific procedures and the sheer volume of services that are provided. It would emphasize less on performing more procedures and ask the question, that frankly patients care about a lot more, which is: what am I getting for those services and how is it helping to preserve or improve my health? I'm very optimistic that this shift will help us move away from certain misaligned incentives unique to a fee for service model. It represents a culture and mindset shift in healthcare as payment reform places more of the financial decision making, but also financial risk on the provider side. It will lead to reducing unnecessary procedures and the misallocation of resources. I invite you to listen or download my complete interview with Dr. Shantanu Agrawal, Deputy Administrator & Director, Center for Program Integrity, Centers for Medicare and Medicaid Services on The Business of Governnent Hour. ******* The Business of Government Radio Show: Conversations with Leaders. What are the key priorities for CMS’s Center for Program Integrity? How is it moving beyond the “pay and chase” approach to combating fraud, waste, and abuse? What innovative technologies is it using? Join host Michael J. Keegan as he explores these questions and more with Dr. Shantanu Agrawal, Deputy Administrator & Director, Center for Program Integrity, Centers for Medicare and Medicaid Services. Broadcast Schedule: The show airs Monday at 11 a.m., and Wednesday at noon, on Federal News Radio 1500AM WFED. If you can't wait, though, you can listen to (or download) this week's program and all our previous interviews at businessofgovernment.org.



